Since 2014, NUWAY used its revenue to subsidize recovery residence support to over 30,000 individuals engaged in clinical care.
The Big Picture
This story illustrates the incredible importance of being afforded due process and the results of a system that penalizes providers with funding cuts before an investigation is conducted.
Addiction remains a leading cause of preventable deaths and poses complex challenges to government officials and treatment providers addressing the crisis.
More details…
The CDC estimates over 94,000 overdose deaths in 2024. While overdose death rates have been declining in recent years, these deaths and the many harms to individuals, families, and communities caused by substance use disorders remain one of America’s leading causes of premature death, trauma, family system problems, isolation, emergency healthcare costs, and lost productivity.
Treating substance use and co-occurring mental health disorders effectively is exceedingly difficult compared to many other chronic medical conditions. Because addiction has biological, psychological, and social components, solutions require a broad range of treatment, environments, employment, training, and other support services.
The opioid epidemic, COVID-19, and rising substance use drastically increased the need for behavioral healthcare. In response, the government relaxed regulations to make it easier for providers and support services to utilize public funds. While saving countless lives, reduced regulation and oversight allowed bad actors to proliferate and take advantage of the system.
More details…
Federal and state governments eased regulatory restrictions to increase the number of available treatment beds and chairs and to make it possible to deliver therapy via telehealth during COVID-19. These changes made it possible for people in active addiction and early recovery to continue receiving vital treatment services and reduced cycles of homelessness, hospitalization, and incarceration.
Easier access to Medicaid (publicly funded healthcare) dollars and looser regulations not only helped well-meaning treatment providers to expand access to care but also made it easier for predators to fraudulently bill the government for hundreds of millions of dollars for treatment and other services that were never delivered.
Federal and state officials and the media have been vigorously pursuing those who knowingly pilfered taxpayer dollars and endangered lives by not delivering vital services. However, investigations that cast too wide a net can inadvertently ensnare good actors along with bad ones.
NUWAY is a 59-year-old cornerstone of Minnesota’s recovery community, delivers evidence-based care to more than 1,000 patients daily, exemplifies a service-based nonprofit mission, and employs some of Minnesota’s finest clinicians.
NUWAY in no way resembles or comports itself like the fraudulent enterprises created to bilk patients and state funding that continue to come to light. NUWAY delivers the treatment it promises, continuously reinvests in improving patient care, provides continuing education, and advances the development and use of best practices. Investigations into NUWAY revolve not around egregious infractions but highly nuanced and unclear billing policies and its practice of ensuring that patients have access to recovery-supportive housing.
These investigations cast high-quality behavioral healthcare providers in an unfair light, could have a chilling effect on the field, and make it harder for those most in need to get the help they deserve. Our hope is for our government counterparts to help all behavioral healthcare providers seek solutions so that they can continue serving Minnesota’s vital behavioral healthcare needs.
NUWAY remains fully transparent and cooperative with its government partners and hopes to engage in a productive process that protects and prioritizes patients.
Who is NUWAY?
NUWAY, founded in 1966, is Minnesota’s largest nonprofit extended behavioral healthcare provider meeting an estimated 13 percent of the state’s treatment needs. Many NUWAY patients experienced homelessness in the six months prior to entering treatment, suffered unresolved trauma and other comorbidities, and lacked supportive family and friend relationships.
In 2023, NUWAY…
Gave $3.4million in charity care
Served 432,807 meals
Provided 15,830 rides to treatment
Trained 95 interns from 27 higher education institutions
Ensured 301,647 nights of safe, sober housing
Treated 7,848 patients
Learn more about NUWAY…
NUWAY is Minnesota’s largest and longest-serving nonprofit behavioral healthcare provider. It was founded in 1966 by members of the Minneapolis Alano Society who realized that people need a safe place to live while seeking recovery from drug and alcohol addiction.
NUWAY’s mission is Recovery In Supportive Environments (R.I.S.E.), a belief and a model of care that aims to ensure that all patients engaged in intensive outpatient treatment can access safe, recovery-supportive housing.
NUWAY operates in Minneapolis, Saint Paul, Rochester, Duluth, St. Cloud, and Mankato, providing evidence-based residential, intensive outpatient, and outpatient treatment for adult substance use and mental health disorders.
In addition to evidence-based treatment for any adult in need, NUWAY connects patients to a complete continuum of care and helps them access available community resources. Most NUWAY patients utilize Medicaid.
Why is NUWAY being investigated?
NUWAY is being investigated for subsidizing clinically indicated recovery housing and for the number of minutes of treatment provided in some group therapy sessions.
Issue One:
Subsidizing Recovery Housing
Fulfilling NUWAY’s Recovery In Supportive Environments (R.I.S.E.) mission means ensuring that people have a safe, secure place to live while engaging in treatment and seeking recovery.
Evidence shows that using recovery residences (sober homes) improves treatment outcomes. These home-like settings are non-medical settings focused on providing a safe and supportive living community that encourages sustained recovery from alcohol and other drug use. Recovery residences are abstinence-based and offer varying degrees of peer support and accountability. There are a variety of these programs that recognize many pathways and philosophies to recovery. They are not “one size fits all.” Some are 12-step-based, some are faith-based, and others incorporate more daily structure.
Because many NUWAY patients have a clinical need for recovery housing and cannot afford its monthly cost, NUWAY uses its revenue, generated by providing evidence-based treatment, to subsidize their recovery residence stay.
The government alleges that subsidizing patient recovery housing is a kickback.
In 2022, the U.S. Department of Justice sent NUWAY a Civil Investigative Demand (CID) — a letter informing NUWAY that its R.I.S.E. model was being investigated. Subsequently, in 2024, two years after the investigation into NUWAY started, the Minnesota Department of Human Services sent a brief letter informing NUWAY that it would stop its Medicaid reimbursements. Because the majority of NUWAY patient care is paid for by Medicaid, stopping these reimbursements would effectively force its closure.
The issue at the center of this investigation is nothing new. Treatment providers in Minnesota have been pairing addiction treatment with housing for over 40 years.
This pairing routinely involves a treatment center providing housing at no cost in a property they own, paying for it via vouchers (as NUWAY does) or billing the government. In each case, the patient is getting housing, but NUWAY’s model offers the patient choice.
NUWAY began partnering with independently operated recovery residences that met quality standards in 2014. NUWAY representatives thoroughly assess each potential partner and maintain communication to ensure that patients receive appropriate services and that housing providers comply with quality practices and standards.
Helping patients find a choice of housing that adheres to quality assurance measures improves the overall quantity and quality of recovery residences statewide.

Recovery housing works.
From 2019 through 2024, NUWAY partnered with the University of Minnesota Center for Practice Transformation to conduct the largest-ever study into the effects of recovery residence utilization on treatment outcomes. Among other benefits, people who use recovery residences during treatment are 30 percent more likely to complete treatment and experience significantly lower depression and anxiety symptoms.
In Summary…
Some assert that offering to subsidize recovery housing for patients who clinically need it but cannot afford it represents an unfair inducement. NUWAY refutes this allegation. Pairing treatment with recovery housing is a wide, long-standing and established practice. Research demonstrates that recovery housing improves treatment outcomes and may reduce long-term care costs. NUWAY is using its resources to fund housing — not charging the government for this service. NUWAY does not receive any form of financial remuneration for these housing subsidy payments, which go fully to independent recovery residence providers. Further, Congress passed a law specifically designed to ensure that healthcare organizations can offer benefits that promote access to care as long as these incentives do not pose a risk of harm to the patient and do not waste government funds. Subsidizing recovery residences improves the overall health and wellness of patients and improves treatment engagement. NUWAY’s payments do not COST the government money; they SAVE it money. Most NUWAY patients are eligible for state housing payments, but those programs can be bureaucratic and difficult to access. NUWAY chooses to spend its money rather than sending patients to the state programs because NUWAY believes that making the process easier for patients is worth it.
IMPORTANT RECOVERY RESIDENCE POLICY UPDATE:
The Governor’s proposed budget, released in January 2025, contains provisions that could completely reshape Minnesota’s recovery residence landscape, decimating housing operators and reducing patient housing access. Read a summary of the proposed changes and potential impacts.
Issue Two:
The Number of Minutes of Group Therapy
The state of Minnesota has a manual that includes instructions for treatment organizations.
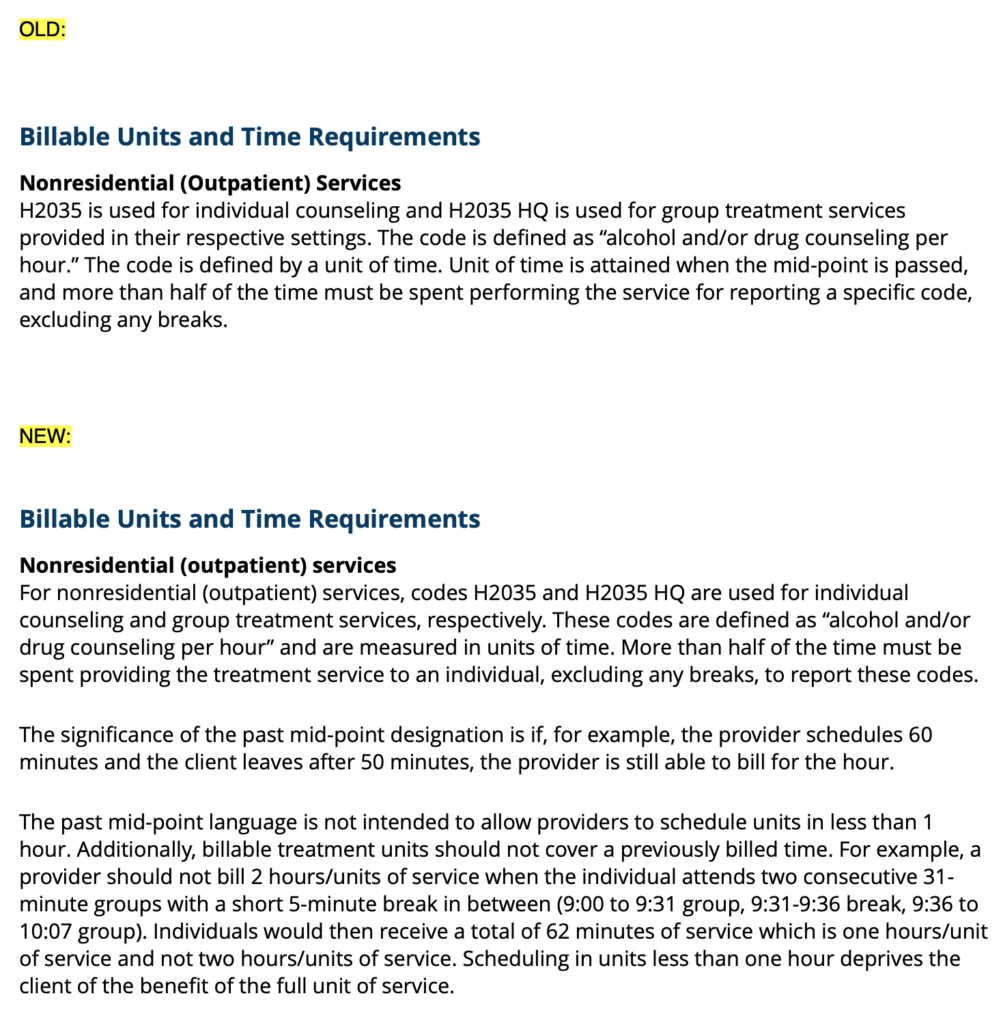
Those instructions are more vague than one might imagine. In the case of billing for intensive outpatient addiction treatment group therapy, the language in place until September 2024 said that providers could bill for one unit of treatment as long as the treatment duration exceeds the mid-point of the time associated with the code. In other words, for a code listed as “sixty minutes,” at least 31 minutes of therapy must be delivered to have a unit of treatment. It is important to note that treatment episodes are billed as “units” and not by time.
While the duration of NUWAY intensive outpatient group therapy sessions differs, some sessions prior to the September 2024 policy change provided approximately 35 minutes of therapy. This has led some to allege that NUWAY was billing for more treatment than it was providing.
This is not the case, however. NUWAY complied with the instructions by providing over 31 minutes of treatment per unit billed.
More importantly, there are clinical reasons for a shorter group therapy duration. Most of the therapy sessions in question were adjusted during COVID-19 to increase telehealth treatment engagement, thereby reducing the number of patients ending sessions early due to screen fatigue.
In short, NUWAY believes that it complies with all regulations and guidance. There were rare situations where a patient was billed for a unit when the patient had left early or arrived late, and no bill should have been generated. NUWAY discovered that error internally and has offered a refund to the government.
Take note of the highlighted language in the 2026-2027 Minnesota Biennial Budget, issued in January 2025.

Please pay particular attention to the first sentence, “Due to the lack of explicit guidance…” It seems the new budget acknowledges that previous policy guidance related to mid-point billing was unclear and led to the possibility of providers beleiving that they were billing appropriately — previous guidance made it impossible to know if an organization was complying with policy.
Another way to look at this allegation…

This graphic illustrates the difference between allegedly fraudulent billing and non-fraudulent billing. The government alleges that treatment units must not be billed within the same hour despite no specific rule language substantiating this assertion. Therefore, billing for two treatment units within the same hour is allegedly fraudulent, while billing for two units in separate hours is not fraudulent. The root of this allegation stems not from the number of units of treatment delivered but from the timing of when these treatment units are delivered throughout the day.
This allegation seems arbitrary, is not stated in Medicaid billing rules of the time, and would make treatment delivery harder for patients and clinicians by reducing schedule flexibility. This illustration should also help dispel the false claim that NUWAY engages in so-called “double-billing,” as alleged in news reporting.
NUWAY is, and has been, fully transparent and cooperative with its government partners during investigations into both issues.
NUWAY has been explicit about subsidizing recovery housing since beginning the practice. In fact, NUWAY described the program in detail to the Commissioner of Human Services. As you can see in this letter, NUWAY stated, “All NUWAY patients are eligible to receive recovery residence subsidization contingent upon weekly treatment compliance reflecting outcome-based goals (sobriety, engagement, behavior, etc.).”
The fact that NUWAY fully disclosed the program to the Commissioner proves that there is no fraud. The fact that no one from the State expressed any concerns to NUWAY indicates that the government believed that the program was legal.
Not only has NUWAY been transparent about its R.I.S.E. model, but some of the state’s largest insurance companies have recognized NUWAY for its recovery residence partnerships and treatment quality.
UCare awarded NUWAY for ensuring that patients access recovery housing.

NUWAY was designated a Blue Distinction® Center for Substance Use Treatment and Recovery by Blue Cross and Blue Shield of Minnesota.
As an evidence-based treatment provider, NUWAY subsidizes recovery housing and adjusts treatment episode durations because these practices produce better clinical outcomes.
All NUWAY programming decisions are implemented to improve measurable outcomes, meet patient needs, and pursue its mission. We believe that it is clear from our work, results, reputation, and broad community relationships that NUWAY is a responsible and upstanding corporate citizen and a vital resource striving for high-quality treatment outcomes.
Our practice of using fee-for-service generated revenue to pay for recovery housing for patients when clinically indicated and alternating our treatment schedule are not the only ways we have found to improve the quality of life and longevity of our patients. NUWAY also provides residential care, offers continuing education to licensed clinicians statewide, pilots new evidence-based treatment modalities, is the largest sponsor of Minnesota recovery events, conducts vital research, and shares insights by presenting at major national conferences.
We choose to do these things not because they financially enrich NUWAY or its dedicated team members (in fact, these activities require the expenditure of substantial NUWAY revenue) but because they serve the needs of clients, improve treatment quality, and serve the charitable mission established 59 years ago.
NUWAY is not just a treatment provider. It is a continuum of care for its patients, maintaining hundreds of relationships to make a broad spectrum of recovery-supportive services accessible because that is what it takes to help many individuals restore health, become independent, and achieve lasting recovery.
What this investigation has already cost NUWAY and its patients…
Complying with this investigation while continuing to deliver treatment has cost NUWAY financial resources that could have gone to providing care.
While NUWAY understands the importance of ensuring regulatory compliance and that investigations like this one are a necessary part of protecting patients and taxpayers, the result has reduced the organization’s ability to meet the needs of as many people as it would like to.
Expansions that would bring much-needed treatment to more parts of Minnesota have been put on hold or brought into question during this process.
Money, time, and resources that could go to helping even more people are being spent instead on legal fees and internal resources needed to address this case.
What could be lost…
So far, the Minnesota Department of Human Services, which controls the state’s Medicaid spending, has granted NUWAY extensions that allow it to continue operating. But NUWAY and those who rely on its services are living in limbo until this matter is settled. Most of them, until now, have not known how close NUWAY has come to having to suspend its services.
Should the government succeed in halting NUWAY’s practice of using its revenue for recovery housing, or if the Minnesota Department of Human Services ceases Medicaid reimbursements, the state will lose approximately 13 percent of its behavioral healthcare capacity within about 30 days. Over 1,000 individuals will need to be transitioned to alternative treatment providers. However, there are not enough providers to meet the needs of these patients, and the threat of homelessness puts recovery into serious question.
The real cost of NUWAY being forced to significantly reduce services or shut down is unmitigated addiction, mental illness, homelessness, incarceration, and preventable deaths.
What can happen to NUWAY can happen to any Medicaid treatment provider, further imperiling our fragile healthcare safety net.
NUWAY supports rooting out and eliminating bad actors preying on patients and taxpayer dollars. After all, the funding they pilfer takes precious resources away from legitimate and vital providers, including NUWAY, who are doing important work to support recovery.
Healthcare regulation is complicated and ever-evolving. Compliance requires skilled experts and careful oversight on the part of providers and their government partners.
Our public healthcare safety net faces a daunting problem if high-quality, compliant providers can be easily tarnished or closed by casting them in the same light as criminal enterprises that purposefully intend to defraud patients and payers. The allegations against NUWAY are complex and nuanced, requiring careful consideration.
Whether news outlets inaccurately portray NUWAY in a negative light or government regulators follow through with threats to defund it, the people who stand to lose the most are individuals and families seeking recovery.